This is an a online e log book to discuss our patient de-identified health data shared after taking his/her/guardians signed informed consent. Here we discuss our individual patients problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problem with collective current best evident based input.
This E blog also reflects my patient centered online learning portfolio and your valuable inputs on the comment box is welcome.
I have been given this case to solve in an attempt to understand the topic of " patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with diagnosis and treatment plan
The patient/ attender was informed the purpose of the information being acquired. An informed consent was taken from patient/ attender and there is omission of information that was requested to be omitt.
Chief complaints:
75 year old female patient was brought to casualty with chief complaints of: C/o shortness of breath since 10 days Bilateral pedal edema since 10 days Facial puffiness since 10 days H/o of palpitation 10 days
HOPI:
Patient was apparently asymptomatic 15 days back & then she developed fever - low grade, intermittent, decreased with Rx
Shortness of breath since 10days which was insidious in onset, gradually progressed from class 2-4, Orthopnea present
C/o palpitations since 10 days B/I pedal edema since 10 days which was
pitting type extending upto knee Facial puffiness present.
No history of chest pain, syncope attack. No history of decreased urine output, abdominal distention. No other complaints
Personal history:
Diet:mixed
Appetite:normal
Bowel and bladder movements:normal
Appetite : decreased
Sleep : adequate
No additions
On examination:-
Pt is C/C/C well oriented to Time ,place and person
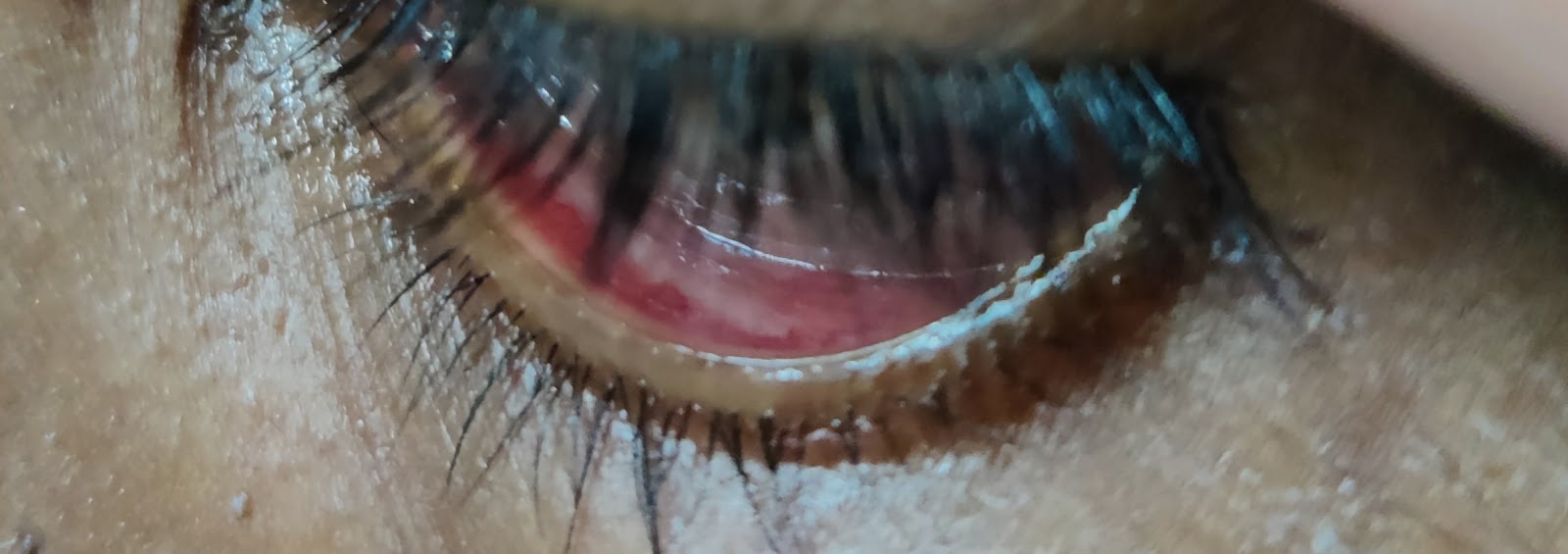
Pallor : present
B/I pedal edema - pitting type extending
upto knees
No cyanosis,clubbing,or generalised lymphadenopathy
Temp: 99F
PR: 130
Bp: 150/90mmhg
RR: 32 cpm
Spo2: 88-92% on RA
CVS:JVP raisedApex beat - diffuse Parasternal heave +Palpable P2 +
S1 S2 +
RS: Barrel shaped chest, Trachea central
BAE+, B/I crepts +
P/A: soft nontender
CNS: NFND
Inspection-
Shape of abdomen normal
Umbilicus -central and inverted
No visible scars,sinuses,dilated veins
Hernial orifices normal
Palpation -no local rise of temperature
No Tenderness present
No guarding,rigidity,rebound tenderness
No hepatomegaly,spleenomegaly
Percussion-
Resonant
Auscultation-
Bowel sounds +
INVESTIGATION:
Serology: Negative
Hemogram:
Serum electrolytes:
LFT:
ABG:
Serum urea:
RBS:
APTT:
:-
2D ECHO
ECG:
ECG at the time of presentation
After Inj. Metaprolol 5 mg IV/stat
26/11/2022
27/11/22
7.00 am
10.00pm
28/11/2022
29/11/2022
30/11/2022
1/12/2022
X-ray:
27 /11/22
28/11/2022
25/11/22
NEW ADMISSION
25/11/2022
S:
75 year old female patient was brought to casualty with chief complaints of: C/o shortness of breath since 10 days Bilateral pedal edema since 10 days Facial puffiness since 10 days H/o of palpitation 10 days
O:PT IS C/C/C
BP-100/70 MM OF HG
PR: 116 BPM RS: BAE+ B/L BASAL CREPTS + IAA, IMA ++
CVS-S1,S2
P/A-SOFT
CNS-NAD
A- ATRIAL FEBRILLATION EITH HEART FAILURE
P:
1 PRBC TRANSFUSION DONE ON 25/11/2022
P:
1.FLUID (1.5 L) & SALT(<2GM) RESTRICTION
2.INJ.LASIX 40 MG IV /BD IF SBP >= 110 MM OF HG
3. T.METXL 25 MG PO/OD
4.T.PAN 40 MG PO/OD
5. T.ECOSPRIN AV 75/10 MG PO/ HS
6. INJ.CLEXANE 40 MG OD / IV
7. T.DOLO 650 MG PO/SOS
8.NEB WITH IPRAVEN 8TH HRLY
BUDECORT
Case uptake from Murali (INTERNEE) TO ME
26/11/2022
26/11/2022
S: 75 year old female patient was brought to casualty with chief complaints of shortness of breath since 10 days Bilateral pedal edema since 10 days Facial puffiness since 10 days H/o of palpitation 10 days
O:PT IS C/C/C
BP-130/70 MM OF HG
PR: 85 BPM
RS:
BAE+
B/L BASAL DIFFUSE CREPTS + IAA, IMA ++
CVS-S1,S2
P/A-SOFT
CNS-NAD
A- ATRIAL FEBRILLATION WITH HEART FAILURE WITH BICYTOPENIA (ANEMIA+THROMBOCYTOPENIA )
P:
1.FLUID (1.5 L) & SALT(<2GM) RESTRICTION
2.INJ.LASIX 40 MG IV /BD IF SBP >= 110
MM OF HG
3. T.METXL 25 MG PO/OD
4.T.PAN 40 MG PO/OD
5. T.ECOSPRIN AV 75/10 MG PO/ HS
6. INJ.CLEXANE 40 MG OD / IV
7. T.DOLO 650 MG PO/SOS
8.NEB WITH IPRAVEN 8TH HRLY
BUDECORT
27/11/2022
S: 75 year old female patient was brought to casualty with chief complaints of shortness of breath since 10 days Bilateral pedal edema since 10 days Facial puffiness since 10 days
PEDAL EDEMA SUBSIDED
SOB DECREASED
FACIAL PUFFINESS DECREASED
O:PT IS C/C/C
BP-110/70 MM OF HG
PR: 120 BPM
RS:BAE+
B/L BASAL DIFFUSE CREPTS + IAA, IMA ++
CVS-S1,S2
P/A-SOFT
CNS-NAD
A- ATRIAL FEBRILLATION WITH HEART FAILURE WITH BICYTOPENIA( ANEMIA+THROMBOCYTOPENIA ) WITH COPD
P:
1.FLUID (1.5 L) & SALT(<2GM) RESTRICTION
2.INJ.LASIX 40 MG IV /BD IF SBP >= 110 MM OF HG
3. T.METXL 25 MG PO/OD
4.T.PAN 40 MG PO/OD
5. T.ECOSPRIN AV 75/10 MG PO/ HS
6. INJ.CLEXANE 40 MG OD / IV
7. T.DOLO 650 MG PO/SOS
8.NEB WITH IPRAVEN 8TH HRLY
BUDECORT
28/11/2022
S: 75 year old female patient was brought to casualty with chief complaints of shortness of breath since 10 days Bilateral pedal edema since 10 days Facial puffiness since 10 days
PEDAL EDEMA SUBSIDED
SOB DECREASED
FACIAL PUFFINESS DECREASED
O:PT IS C/C/C
BP-80/50 MM OF HG
PR: 141 BPM
RS:
BAE+
B/L BASAL DIFFUSE CREPTS +
CVS-S1,S2
P/A-SOFT ,NIN TENDER
CNS-NAD
A- ATRIAL FEBRILLATION WITH HEART FAILURE WITH BICYTOPENIA(ANEMIA+THROMBOCYTOPENIA ) WITH VOPD
1 PRBC TRANSFUSION DONE ON 25/11/2022
P:
1.FLUID (1.5 L) & SALT(<2GM) RESTRICTION
2.INJ.LASIX 40 MG IV /BD IF SBP >= 110 MM OF HG
3. T.METXL 25 MG PO/OD
4.T.PAN 40 MG PO/OD
5. T.ECOSPRIN AV 75/10 MG PO/ HS
6. INJ.CLEXANE 40 MG OD / IV
7. T.DOLO 650 MG PO/SOS
8.NEB WITH IPRAVEN 8TH HRLY
BUDECORT
29/11/2022
75/F with PEDAL EDEMA & SOB
D.O.A: 24/11/11
S:
PEDAL EDEMA SUBSIDED
SOB DECREASED
O:
PT IS C/C/C
BP-110/70 MM OF HG
PR: 100 - 130 BPM IRREGULARLY IRREGULAR
RS:
BAE+
B/L BASAL CREPTS +
CVS-S1,S2
P/A-SOFT ,NON TENDER
CNS-NAD
A- ATRIAL FIBRILLATION WITH HEART FAILURE
COPD
BICYTOPENIA (ANEMIA+THROMBOCYTOPENIA) ?B12 DEFICIENCY
1 PRBC TRANSFUSION DONE ON 25/11/2022
P:
1.FLUID (1.5 L) & SALT(<2GM) RESTRICTION
2.INJ.LASIX 40 MG IV /BD IF SBP >= 110 MM OF HG
3. T.METXL 25 MG PO/BD
4. T.ECOSPRIN AV 75/10 MG PO/ HS
6. INJ.CLEXANE 40 MG SC/OD
7. T.WARFARIN 2 MG PO/OD @ 6.00 PM
8. T.DOLO 650 MG PO/SOS
9.NEB WITH IPRAVEN 8TH HRLY
BUDECORT